A positive urine culture is based on the growth of bacteria in a large number of colony forming units (CFU).
Urine culture results should be interpreted in conjunction with clinical symptoms of urinary tract infection (UTI), such as dysuria, urinary frequency, suprapubic pain, flank pain, and fever. For clean collection urine samples, a positive urine culture indicated by bacterial growth greater than 100,000 CFU / ml is suggestive of UI; a growth of 1,000-100,000 CFU / mL can still indicate a UTI, especially for a sample taken at cystoscopy or other invasive procedures.
The reliability of the results is determined by the quality of the sample and the collection, transportation and handling of the sample to the laboratory.
The growth of 2 or more different bacteria or polymicrobial growth is likely the result of contamination.
A positive urine culture is further tested to identify the organism and test its susceptibility to antibiotics, in order to guide antimicrobial therapy, if necessary.
Clean Voided Specimen
- Normal: <10,000 organisms per ml
- Urinary Tract Infection
- Boys
- Organisms >10,000 per ml suggests UTI likely
- Girls
- Organisms >100,000 per ml suggests UTI
- Three specimens: 95% probability of UTI
- Two specimens: 90% probability of UTI
- One specimen: 80% probability of UTI
- Organisms >10,000 per ml needs repeat Urine Culture
- Organisms >100,000 per ml suggests UTI
- Boys
Transurethral Catheterization
- Normal: <1,000 organisms per ml
- Urinary Tract Infection
- Organisms >10,000 per ml suggests UTI
- Organisms >1,000 per ml needs repeat Urine Culture
Suprapubic aspiration in infants
- Gram Negative Bacilli: any number suggests UTI (99%)
- Gram Positive Cocci: >1-2,000 suggests UTI (99%)
Normal Values
| Negative | <10,000 colonies/ml |
| Indeterminate | 10,000-100,000 colonies/ml |
| Positive | >100,000 colonies/ml |
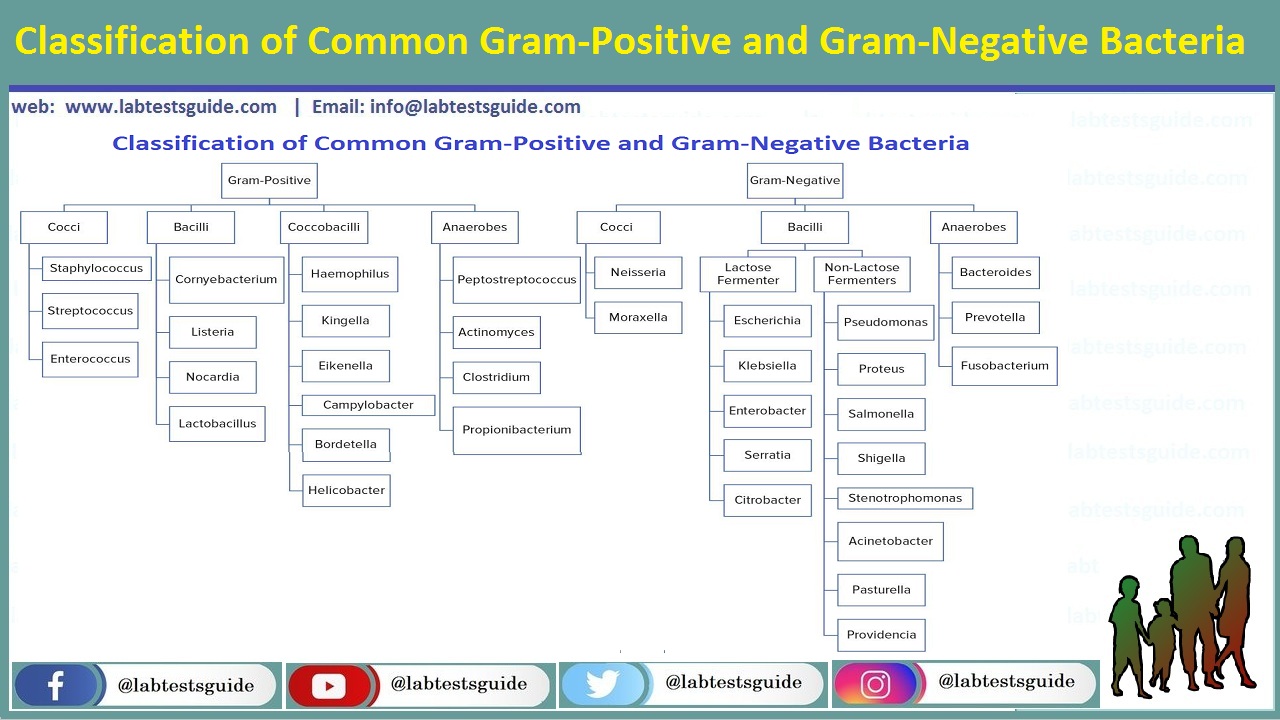
Common Uropathogens
- Escherichia coli
- Other Enterobactoe
- Klebsiella pneumoniae
- Enterobacter
- Proteus mirabilis
- Citrobacter
- Pseudomonas aeruginosa
- Enterococcus
- Staphylococcus saprophyticus
- Staphylococcus aureus
- Streptococcus agalactiae
- Candida
Uncommon Uropathogens:
- Corynebacterium urealyticum
- Haemophilus influenzae and H parainfluenzae
- Blastomyces dermatitidis
- Neisseria gonorrhoeae
- Mycobacterium tuberculosis
Escherichia coli:
- E. coli is gram-negative
- Catalase Positive
- Citrate Negative
- Oxidase Negative
- Coagulase Negative
- Growth on 15-45°C.
- Pigment Negative
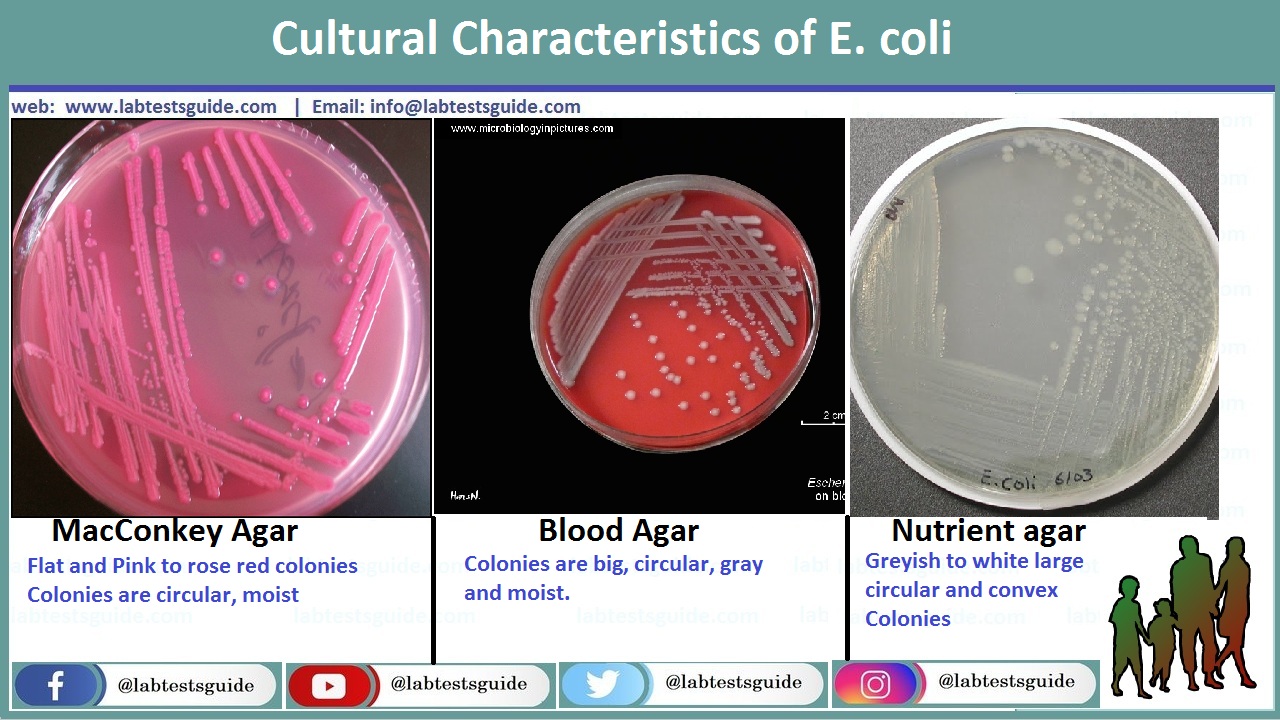
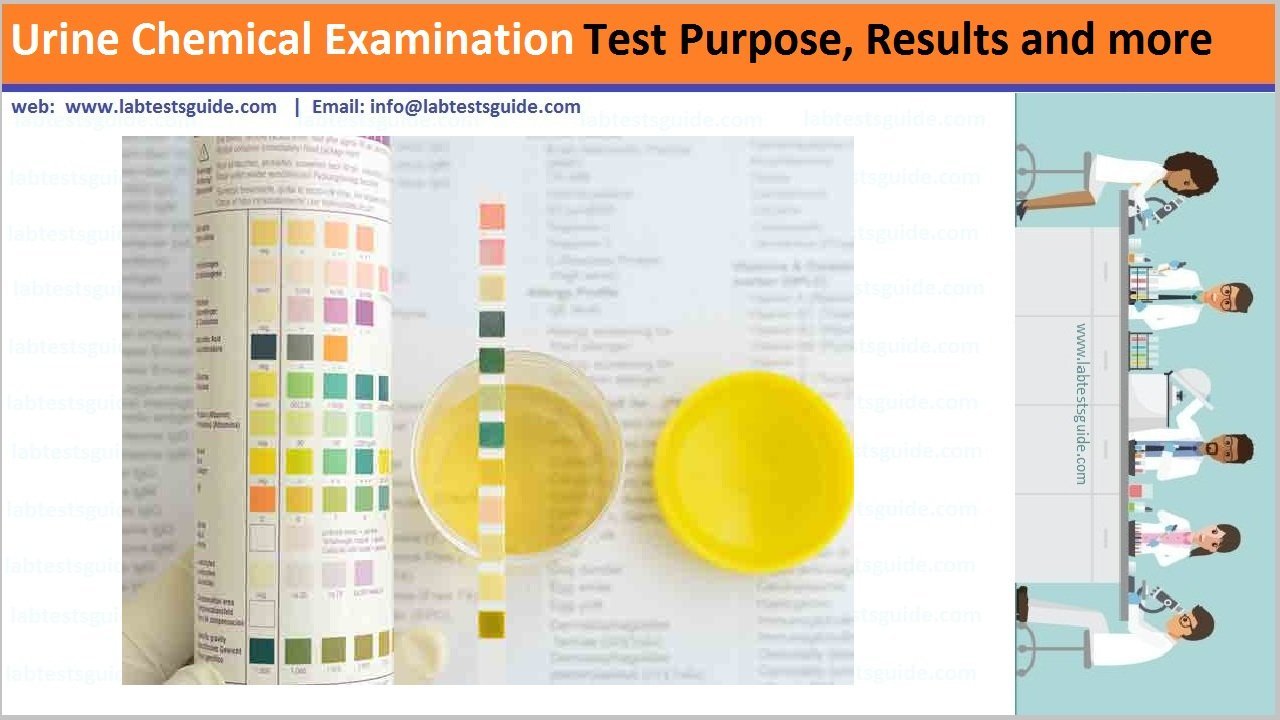
- MacConkey Agar: Pink to rose red colonies (may be surrounded by a zone of precipitated bile)
- Nutrient agar: Greyish to white-colored large, circular and convex colonies; smooth and rough colonies.
- Blood Agar: Colonies are big, circular, gray and moist.
- Lactose: They give lactose positive yellow colonies.
Pseudomonas aeruginosa
- Gram-negative
- Catalase Positive
- Citrate Negative
- Oxidase Positive
- Coagulase Negative
- Growth on 15-45°C.
- Pigment: Positive (Blue/Green)

- MacConkey Agar: Irregular, colorless to pink colonies
- Nutrient agar: Greenish blue (due to pigment production)
- Blood Agar: Greyish white
Enterococcus:
- Gram-Positive
- Catalase Negative
- Citrate Negative
- Growth on 15-45°C.
- Pigment: Negative
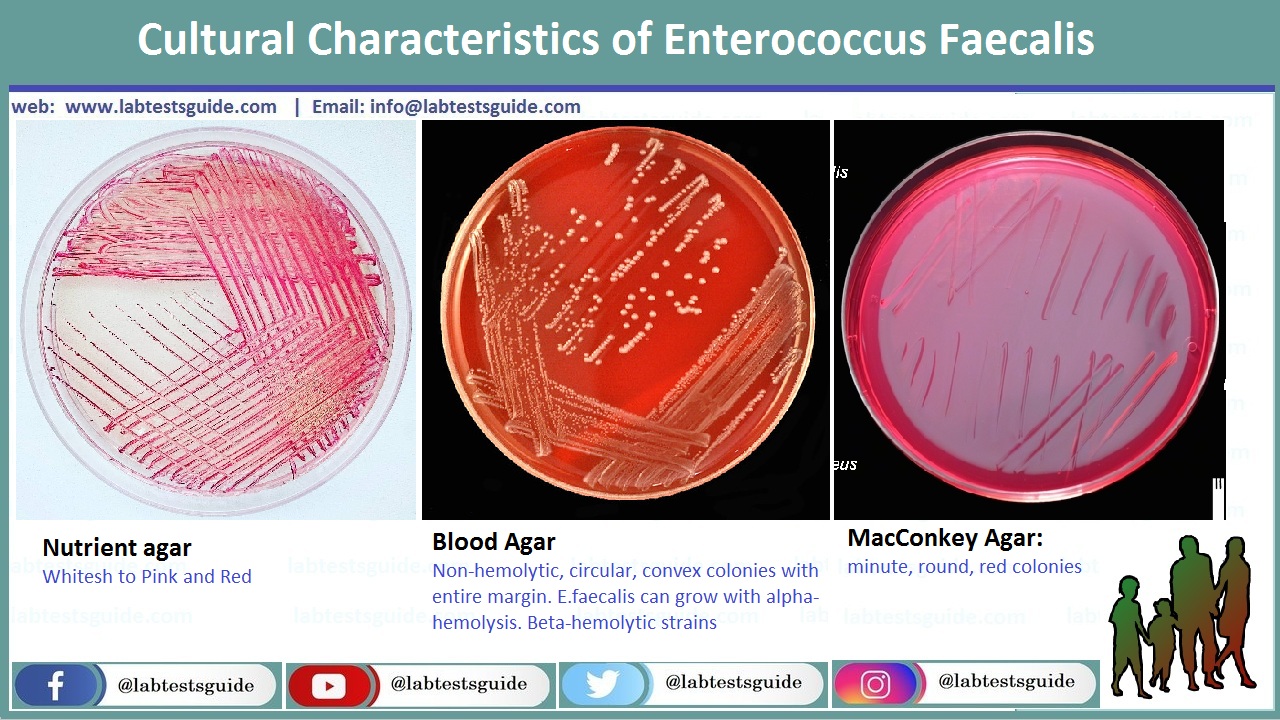
- MacConkey Agar: minute, round, red colonies
- Nutrient agar: Colorless Whitesh
- Blood Agar: Non-hemolytic, circular, convex colonies with entire margin. E.faecalis can grow with alpha-hemolysis. Beta-hemolytic strains
Staphylococcus saprophyticus:
- Gram-Positive
- Catalase Positive
- Citrate Positive
- Oxidase Negative
- Coagulase Positive
- Growth on 15-45°C.
- Pigment golden yellow
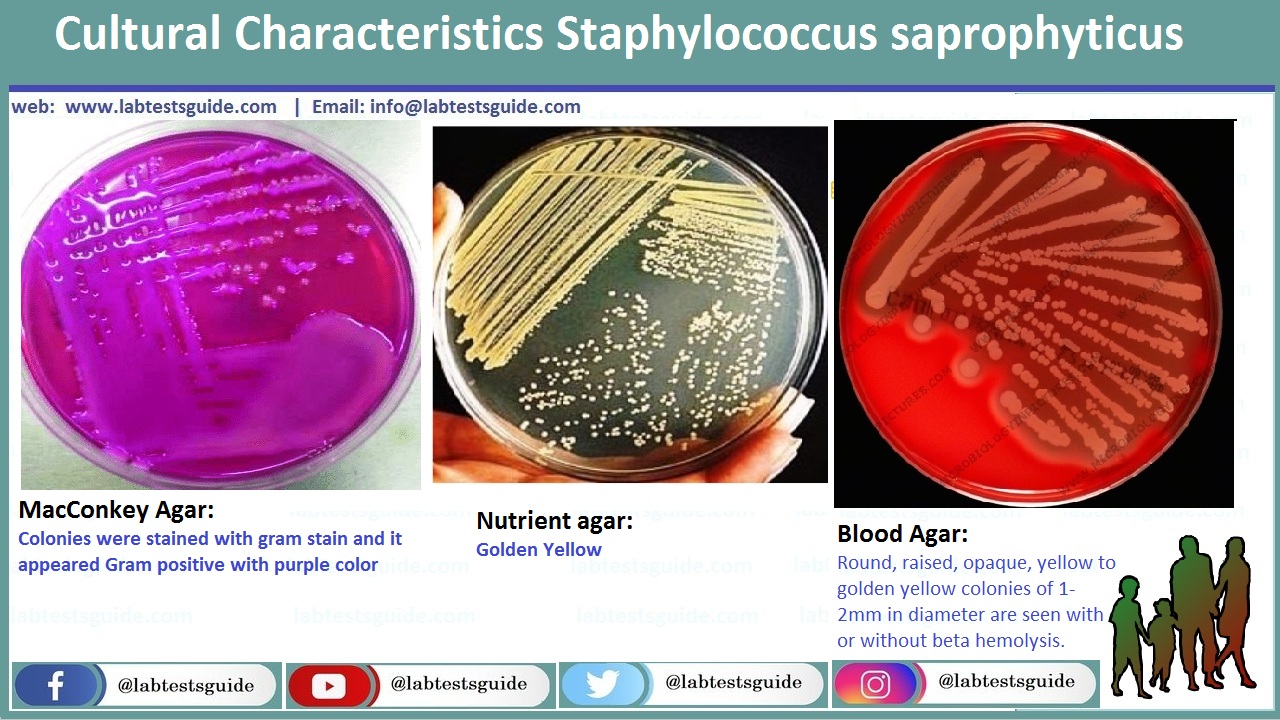
- MacConkey Agar: colonies were stained with gram stain and it appeared Gram positive with purple color
- Nutrient agar: Golden Yellow
- Blood Agar: Round, raised, opaque, yellow to golden yellow colonies of 1-2mm in diameter are seen with or without beta hemolysis.
Related Articles:
RELATED POSTS
View all