Staphylococcus aureus, a frequent colonizer of the skin and mucosa of humans and animals, is a highly successful opportunistic pathogen.
Staphylococcus aureus are Gram-positive, singly, in pairs, or in a short chain of 3-4 bacteria. They are Catalase positive, Oxidase negative.
Habitat of Staphylococcus aureus
- The natural habitat is the body surfaces of mammals.
- They are normal flora of the skin and mucous membranes.
- Also present in the nose / anterior nostrils.
- They can also be found in Pharynx.
- It is found in stratified epithelial cells or in mucosal or serum components associated with these cells.
- It is found in the skin / nasal passages and armpits of humans.
- They act as a benign or symbiotic relationship with the hosts.
- Enterogeneric strains of S. aureus are found in various food products.
- They can survive on dry skin.
- Thirty percent (30%) of the normal healthy human population is affected by S. aureus, as it asymptomatically colonizes the skin of the human host.
Staphylococcus aureus morphology
- Gram-positive, alone, in pairs or in a short chain of 3-4 bacteria.
- Irregular cell groupings.
- 1 um diameter
- Spherical colonies grouped in two planes.
- Cell wall: very thick peptidoglycan layer
- Not flagellated, not mobile and without spores
- They are encapsulated.
- Grapes as a cluster arrangement.
Virulence factors:
- Surface proteins: Protein A (prevents Complement activation), Agglutination factor, Teichoic acid (adhesion and induction of septic shock)
- Super Antigens: Enterotoxin A-D, Exfoliatin A&B, Super Antigen of Toxic Shock Syndrome Toxin (TSST).
- Cytotoxins: α-hemolysin, β-hemolysin, γ-hemolysin, δ-hemolysin, Panton Valentine Leucocidin (PVL), Exfliatin (epidermolytic-cleaves desmglein in desmosomes)
- Enzymes: nuclease, lipase, hyaluronidase, coagulase (causes plasma to clot), staphylokinase, glycerol ester hydrolase, catalase (degradation of H2O2 limits the ability of neutrophils to kill S. aurues), etc.
Laboratory diagnosis
1. Gram staining:
Gram positive cocci in clusters is the characteristics, cocci may appear singly in pairs or in short chains.
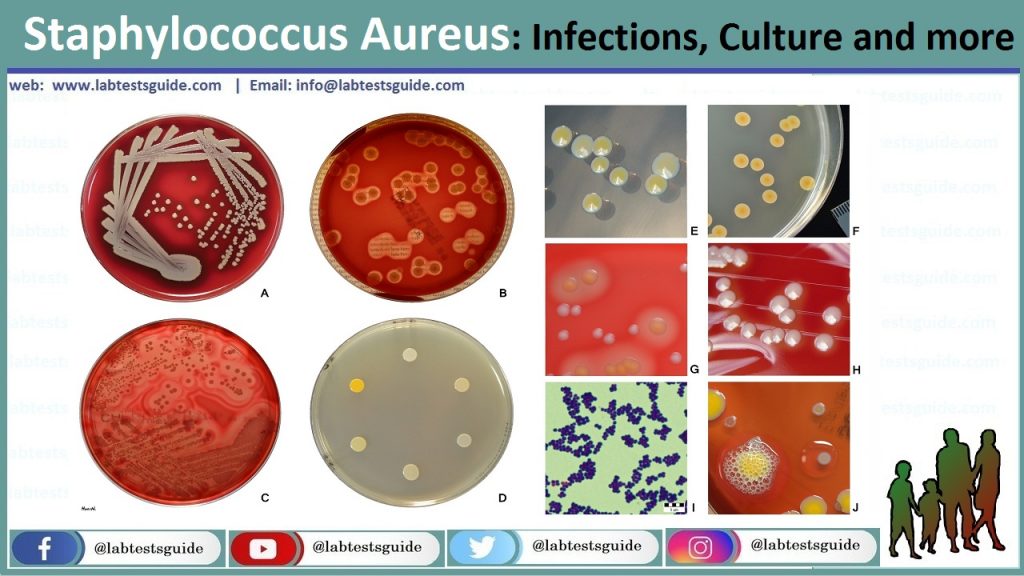
2. Culture:
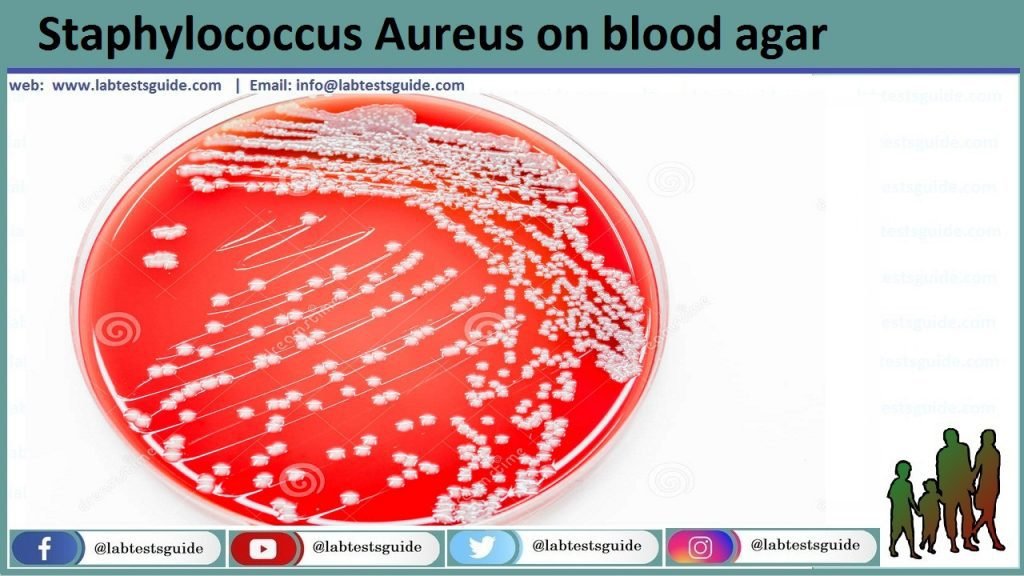
- Blood Agar: growth occurs abundantly within 18 to 24 hours, yellow or golden yellow colonies with or without Beta hemolysis are seen.
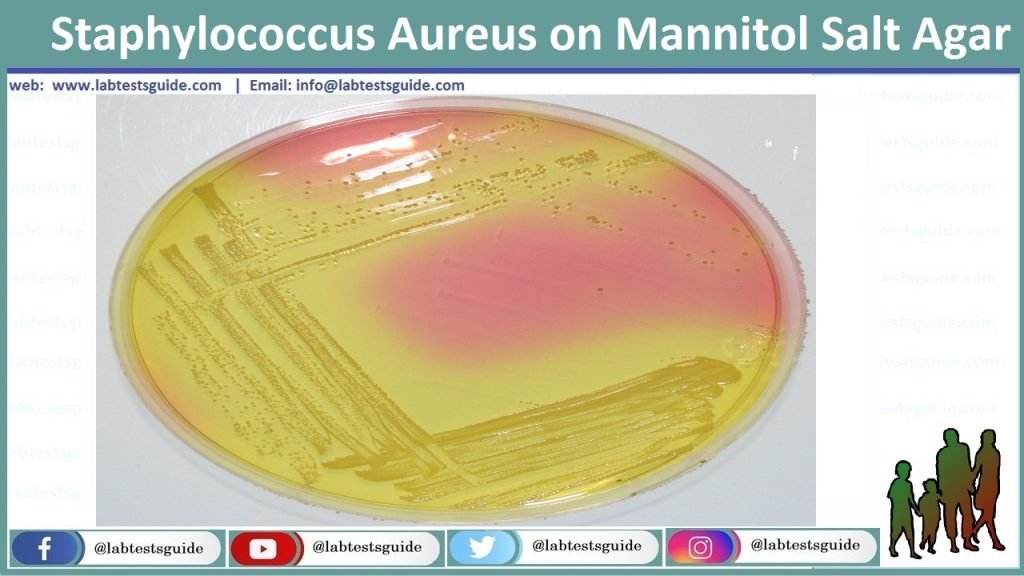
- Mannitol Salt Agar (MSA) is a selective media commonly used for the isolation of S. aureus.
After inoculation, MSA plates were incubated at 35°C for 24 to 48 hours. S. aureus is Mannitol fermenting bacteria and gives yellow or gold colonies.
3. Biochemical tests:
- Catalase test: Positive
- Coagulase test: Positive- Distinguish S. aureus from coagulase-negative Staphylococcus aureus (CONS). CONS are further differentiated on the basis of Novobiocin sensitivity test ( S. epidermidis is sensitive, whereas S. saprophyticus is resistant).
Who gets S. aureus infections?
Anyone can develop a S. aureus infection, although certain groups of people are more likely than others. This includes people with conditions such as: diabetes, cancer, vascular disease, eczema, lung disease, and people who inject drugs. Patients who are hospitalized in intensive care units (ICUs), patients who have undergone certain types of surgeries, and patients with medical devices inserted in their bodies, such as central lines and catheters, are at greater risk of a more serious S. aureus infection. People who often visit healthcare facilities and nursing home residents are also at an increased risk.
Symptoms of S. aureus infections?
S. aureus infections typically appear on the skin as a pocket of pus surrounded by red, painful skin, or cellulitis.
Main diseases caused by Staphylococcus aureus
- Skin Infections & Surgical wound infections
- Osteomyelitis
- Food poisoning/gastroenteritis
- Toxic shock syndrome
- Pneumonia (mainly hospital acquired)
- Acute endocarditis
- Infective arthritis
- Necrotizing fasciitis
- Sepsis and Staphylococcal scalded skin syndrome (SSSS)
Biochemical Test of Staphylococcus aureus
| Basic Characteristics | Staphylococcus aureus |
|---|---|
| Capsule | Non-Capsulated |
| Catalase | Positive (+ve) |
| Citrate | Positive (+ve) |
| Coagulase | Positive (+ve) |
| Gas | Negative (-ve) |
| Gelatin Hydrolysis | Positive (+ve) |
| Gram Staining | Positive (+ve) |
| H2S | Negative (-ve) |
| Hemolysis | Positive (+ve)- Beta |
| Indole | Negative (-ve) |
| Motility | Negative (-ve) |
| MR (Methyl Red) | Positive (+ve) |
| Nitrate Reduction | Positive (+ve) |
| OF (Oxidative-Fermentative) | Fermentative |
| Oxidase | Negative (-ve) |
| Pigment | Mostly Positive (+ve) |
| PYR | Negative (-ve) |
| Shape | Cocci |
| Spore | Non-Sporing |
| Urease | Positive (+ve) |
| VP (Voges Proskauer) | Positive (+ve) |
| Arabinose | Negative (-ve) |
| Cellobiose | Negative (-ve) |
| DNase | Positive (+ve) |
| Fructose | Positive (+ve) |
| Galactose | Positive (+ve) |
| Glucose | Positive (+ve) |
| Lactose | Positive (+ve) |
| Maltose | Positive (+ve) |
| Mannitol | Positive (+ve) |
| Mannose | Positive (+ve) |
| Raffinose | Negative (-ve) |
| Ribose | Positive (+ve) |
| Salicin | Negative (-ve) |
| Sucrose | Positive (+ve) |
| Trehalose | Positive (+ve) |
| Xylose | Negative (-ve) |
| Acetoin Production | Positive (+ve) |
| Alkaline Phosphatase | Positive (+ve) |
| Arginine Dehydrolase | Positive (+ve) |
| Hyalurodinase | Positive (+ve) |
| Lipase | Positive (+ve) |
| Ornithine Decarboxylase | Negative (-ve) |
Prevention of Staphylococcus aureus infection
- Proper wound cleaning and the use of disinfectants help prevent infection.
- Thorough hand washing and covering exposed skin help medical personnel prevent infection or spread to other patients.
- Patients and staff carrying epidemic strains, particularly MRSA, should be isolated.
- Patients can be given disinfectant baths or treated with a topical antibiotic to eradicate the transport of MRSA.
- Infection control programs should be used in hospitals.
Treatment of Staphylococcus aureus infection
- Localized infections are treated by incision and drainage, while antibiotic therapy is indicated for systemic infections.
- Oral therapy may include trimethoprim-sulfamethoxazole, doxycycline or minocycline, clindamycin, or linezolid; Vancomycin is the drug of choice for intravenous therapy, with daptomycin, tigecycline, or linezolid as acceptable alternatives.
- Methicillin-resistant Staphylococcus aureus (MRSA) infections acquired in the hospital and in the community are a major global problem. Therefore, empirical therapy should include antibiotics active against MRSA strains.
- Treatment is symptomatic for patients with food poisoning (although the source of infection must be identified so that appropriate preventive procedures can be implemented)
Related Articles:
Keywords: aureus, lab diagnosis of staphylococcus aureus, staphylococci, staphylococcus, staphylococcus (disease cause), staphylococcus aureus, staphylococcus aureus (disease cause), staphylococcus aureus infections, staphylococcus aureus microbiologia, staphylococcus aureus microbiology, staphylococcus aureus pathogenicity, staphylococcus aureus pronunciation, staphylococcus epidermidis, staphylococcus saprophyticus
RELATED POSTS
View all