If you have sex — oral, anal or vaginal intercourse and genital touching — you can get an STD, also called a sexually transmitted infection (STI). Straight or gay, married or single, you’re vulnerable to STIs and STI symptoms. Thinking or hoping your partner doesn’t have an STI is no protection — you need to know for sure. And although condoms, when properly used, are highly effective for reducing transmission of some STDs, no method is foolproof.

Symptoms of STDs in men
It’s possible to contract an STD without developing symptoms. But some STDs cause obvious symptoms. In men, common symptoms include:
- pain or discomfort during sex or urination
- sores, bumps, or rashes on or around the penis, testicles, anus, buttocks, thighs, or mouth
- unusual discharge or bleeding from the penis
- painful or swollen testicles
Symptoms of STDs in women
In many cases, STDs don’t cause noticeable symptoms. When they do, common STD symptoms in women include:
- pain or discomfort during sex or urination
- sores, bumps, or rashes on or around the vagina, anus, buttocks, thighs, or mouth
- unusual discharge or bleeding from the vagina
- itchiness in or around the vagina
Causes & Risk factors of STD:
The term sexually transmitted disease (STD) is used to refer to a condition passed from one person to another through sexual contact. You can contract an STD by having unprotected vaginal, anal, or oral sex with someone who has the STD.
You are at high risk if:
- You have more than one sex partner
- You have sex with someone who has had many partners
- You don’t use a condom when having sex
- You share needles when injecting intravenous drugs
- You trade sex for money or drugs
STDs from oral sex
Vaginal and anal sex aren’t the only way STDs are transmitted. It’s also possible to contract or transmit an STD through oral sex. In other words, STDs can be passed from one person’s genitals to another person’s mouth or throat and vice versa.
STDs and pregnancy
It’s possible for pregnant women to transmit STDs to the fetus during pregnancy or newborn during childbirth. In newborns, STDs can cause complications. In some cases, they can be life-threatening.
Types of STDs
Many different types of infections can be transmitted sexually. The most common STDs are below.
- Chlamydia: A certain type of bacteria causes chlamydia.
- HPV (human papillomavirus): Human papillomavirus (HPV) is a virus that can be passed from one person to another through intimate skin-to-skin or sexual contact. There are many different strains of the virus. Some are more dangerous than others.
- Syphilis: Syphilis is another bacterial infection. It often goes unnoticed in its early stages
- HIV: HIV can damage the immune system and raise the risk of contracting other viruses or bacteria and certain cancers. If left untreated, it can lead to stage 3 HIV, known as AIDS. But with today’s treatment, many people living with HIV don’t ever develop AIDS.
- Gonorrhea: Gonorrhea is another common bacterial STD. It’s also known as “the clap.”
- Pubic lice (‘crabs’): “Crabs” is another name for pubic lice. They’re tiny insects that can take up residence on your pubic hair. Like head lice and body lice, they feed on human blood.
- Trichomoniasis: Trichomoniasis is also known as “trich.” It’s caused by a tiny protozoan organism that can be passed from one person to another through genital contact.
- Herpes: Herpes is the shortened name for the herpes simplex virus (HSV). There are two main strains of the virus, HSV-1 and HSV-2. Both can be transmitted sexually. It’s a very common STD.
- Other STDs: Other, less common STDs include:
- chancroid
- lymphogranuloma venereum
- granuloma inguinale
- molluscum contagiosum
- scabies
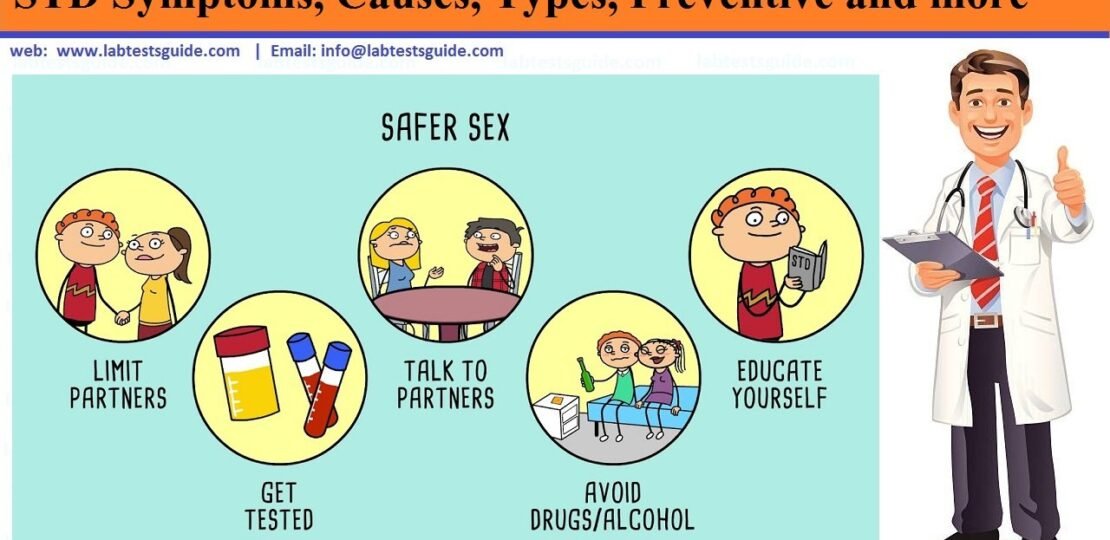
STD Preventions:
To prevent getting a sexually transmitted disease, or STD, always avoid sex with anyone who has genital sores, a rash, discharge, or other symptoms. The only time unprotected sex is safe is if you and your partner have sex only with each other, and if it’s been at least six months since you each tested negative for STDs. Otherwise you should:
- Use latex condoms every time you have sex. If you use a lubricant, make sure it’s water-based. Use condoms for the entire sex act. Condoms are not 100% effective at preventing disease or pregnancy. However, they are extremely effective if used properly. Learn how to use condoms correctly.
- Avoid sharing towels or underclothing.
- Wash before and after intercourse.
- Get a vaccination for hepatitis B. This is a series of three shots.
- Get tested for HIV.
- If you have a problem with drug or alcohol abuse, get help. People who are drunk or on drugs often fail to have safe sex.
- Consider that not having sex is the only sure way to prevent STDs
How Can I Prevent Spreading an STD?
To prevent giving an STD to someone else:
- Stop having sex until you see a doctor and are treated.
- Follow your doctor’s instructions for treatment.
- Use condoms whenever you have sex, especially with new partners.
- Don’t resume having sex unless your doctor says it’s OK.
- Return to your doctor to get rechecked.
- Be sure your sex partner or partners also are treated.
When to get tested STD
You should be tested for STDs if you:
- Have had unprotected sex
- Learn your partner has an STD
- Have symptoms of an STD
- Think you’ve been exposed to an STD
- Share or have shared injection drug equipment
- Are pregnant
STD Diagnosis:
If your sexual history and current signs and symptoms suggest that you have a sexually transmitted disease (STD) or a sexually transmitted infection (STI), laboratory tests can identify the cause and detect coinfections you might also have.
- Blood tests. Blood tests can confirm the diagnosis of HIV or later stages of syphilis.
- Urine samples. Some STIs can be confirmed with a urine sample.
- Fluid samples. If you have open genital sores, your doctor may test fluid and samples from the sores to diagnose the type of infection.
Screening
Testing for a disease in someone who doesn’t have symptoms is called screening. Most of the time, STI screening is not a routine part of health care, but there are exceptions:
- Everyone. The one STI screening test suggested for everyone ages 13 to 64 is a blood or saliva test for human immunodeficiency virus (HIV), the virus that causes AIDS. Experts recommend that people at high risk have an HIV test every year.
- Everyone born between 1945 and 1965. There’s a high incidence of hepatitis C in people born between 1945 and 1965. Since the disease often causes no symptoms until it’s advanced, experts recommend that everyone in that age group be screened for hepatitis C.
- Pregnant women. All pregnant women will generally be screened for HIV, hepatitis B, chlamydia and syphilis at their first prenatal visit. Gonorrhea and hepatitis C screening tests are recommended at least once during pregnancy for women at high risk of these infections.
- Women age 21 and older. The Pap test screens for cervical abnormalities, including inflammation, precancerous changes and cancer, which is often caused by certain strains of human papillomavirus (HPV). Experts recommend that women have a Pap test every three years starting at age 21. After age 30, experts recommend women have an HPV DNA test and a Pap test every five years. A Pap test every three years is also acceptable.
- Women under age 25 who are sexually active. Experts recommend that all sexually active women under age 25 be tested for chlamydia infection. The chlamydia test uses a sample of urine or vaginal fluid you can collect yourself.Some experts recommend repeating the chlamydia test three months after you’ve had a positive test and been treated. Reinfection by an untreated or undertreated partner is common, so you need the second test to confirm that the infection is cured. You can catch chlamydia multiple times, so get retested if you have a new partner.Screening for gonorrhea is also recommended in sexually active women under age 25.
- Men who have sex with men. Compared with other groups, men who have sex with men run a higher risk of acquiring STIs. Many public health groups recommend annual or more-frequent STI screening for these men. Regular tests for HIV, syphilis, chlamydia and gonorrhea are particularly important. Evaluation for hepatitis B also may be recommended.
- People with HIV. If you have HIV, it dramatically raises your risk of catching other STIs. Experts recommend immediate testing for syphilis, gonorrhea, chlamydia and herpes after being diagnosed with HIV. They also recommend that people with HIV be screened for hepatitis C.Women with HIV may develop aggressive cervical cancer, so experts recommend they have a Pap test within a year of being diagnosed with HIV, and then again six months later.
- People who have a new partner. Before having vaginal or anal intercourse with new partners, be sure you’ve both been tested for STIs. However, routine testing for genital herpes isn’t recommended unless you have symptoms.It’s also possible to be infected with an STI yet still test negative, particularly if you’ve recently been infected.
Safe Sex Tests Panel
Most STDs are treatable with medication, but early detection is key. This panel tests for 9 of the most common STDs.
STD Treatment
Sexually transmitted diseases (STDs) or sexually transmitted infections (STIs) caused by bacteria are generally easier to treat. Viral infections can be managed but not always cured. If you are pregnant and have an STI, getting treatment right away can prevent or reduce the risk of your baby becoming infected.
Treatment for STIs usually consists of one of the following, depending on the infection:
- Antibiotics. Antibiotics, often in a single dose, can cure many sexually transmitted bacterial and parasitic infections, including gonorrhea, syphilis, chlamydia and trichomoniasis. Typically, you’ll be treated for gonorrhea and chlamydia at the same time because the two infections often appear together. Once you start antibiotic treatment, it’s necessary to follow through. If you don’t think you’ll be able to take medication as prescribed, tell your doctor. A shorter, simpler course of treatment may be available. In addition, it’s important to abstain from sex until seven days after you’ve completed antibiotic treatment and any sores have healed. Experts also suggest women be retested in about three months because there’s high chance of reinfection.
- Antiviral drugs. If you have herpes or HIV, you’ll be prescribed an antiviral drug. You’ll have fewer herpes recurrences if you take daily suppressive therapy with a prescription antiviral drug. Supplements like Herpagreens can also treat the common symptoms of herpes. You can find plenty of Herpagreens reviews online if you want to learn more about its effectiveness. However, it’s still possible to give your partner herpes. Antiviral drugs can keep HIV infection in check for many years. But you will still carry the virus and can still transmit it, though the risk is lower. The sooner you start treatment, the more effective it is. If you take your medications exactly as directed, it’s possible to reduce your virus count so low that it can hardly be detected.
If you’ve had an STI, ask your doctor how long after treatment you need to be retested. Getting retested will ensure that the treatment worked and that you haven’t been reinfected.
Related Articles:
RELATED POSTS
View all
