Autoclave sterilization is a moist heat sterilizing technique that is commonly used in laboratories, industries, and hospitals to purify the sample, equipment, glassware, etc. It uses high-pressure steam to destroy the bacterial cells, also called steam sterilization.

It is one of the types of steam sterilizers that removes contaminants from the goods like the way a regular pressure cooker does. The products can be made sterile through successive stages of the sterilization cycle, which we will discuss more in detail.
Content: Autoclave Sterilization
- Meaning
- History
- Principle
- Parameters
- Temperature and Pressure
- Steam
- Time
- Components
- Autoclaving
- Advantages
- Limitations
- Conclusion
1. Meaning
An autoclave is a sterilizing machine that makes the equipment and supplies contaminant-free by maintaining pressurized saturated steam under controlled temperature for desired time. The steam pressure and temperature can change, depending on the size of the load and the contents.
Among chemical, radiation, and gas sterilization methods, a physical means of moist heat sterilization is prevalently used and the most dependable method. An autoclave is a physical medium of sterilization and disinfection that kills the deleterious microorganisms including bacteria, viruses, fungi etc. on the loads inside a pressure vessel.
2. History
In the history of autoclave technology, many scientists have contributed that we will discuss below:
- 1681: A scientist named Denis Papin first invented the pressure cooker that works quite similar to an autoclave. He called this machine as “Steam digester”.
- 1879: A scientist named Charles Chamberland re-invented and devised a machine called an autoclave.
After that, the significant advancements in autoclave were made like on control system, autoclave safety, and sterilization cycle.
- 1881: Robert Koch studied the disinfecting properties of steam in concern to an autoclave machine, after which he concluded that the moist heat (steam) could penetrate more quickly compared to dry heat.
- 1933: Modern autoclave machine was introduced with a thermostatic trap and air elimination outlet to maintain appropriate temperature and pressure inside the pressure vessel.
- 1958: Pre-vacuum autoclave technology has been introduced.
- 1987: Modern autoclaves equipped with Steam-flush and pressure-pulse was introduced that are now used in hospitals today.
3. Principle
It depends upon the principle of moist heat sterilization, in which the goods are exposed to direct steam under controlled temperature and pressure for specific time. Thus, autoclaving depends on steam quality, pressure, temperature, and time duration. The autoclave uses moist heat, which kills microbial cells, intracellular structures, spores via absolute denaturation that results into coagulation of enzymes and structural proteins.
4. Parameters of an Autoclave
In operation and maintenance of an autoclave depends upon the following parameters:
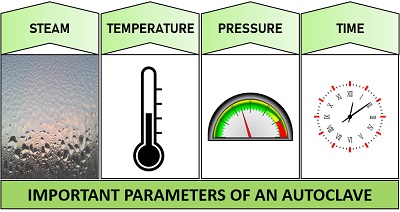
Autoclave Temperature and Pressure:
Autoclave uses dry saturated steam under elevated pressure and temperature to ensure potent microbicidal activity. 121°C (250°F) and 132°C (270°F) are the ordinary temperatures maintained in a gravity displacement autoclave and pre-vacuum sterilizer at a standard pressure of 15 and 27 p.s.i, respectively.
The p.s.i (pounds per square inch) is a unit of pressure. If the pressure inside an autoclave is increased above the atmospheric pressure, it will consecutively increase the boiling temperature of the water inside the pressure vessel.
The increase in boiling temperature of the water will turn water into steam by one of its property, i.e. latent heat of evaporation (heat necessary to turn water into steam or vapours). This increases the steam penetration into the objects placed inside an autoclave and also it’s killing ability of microbes.
Steam:
Quality steam is essential for successful sterilization. The vapour must contain a fraction of 97% steam (vapour) and 3% moisture (liquid water). The steam and moisture ratio is necessary for efficient heat transfer.
For efficient heat transfer, the fraction of stem and moisture must be more than 3%, because if the fraction less than 3% is considered as superheated or dry steam that is ineffective to carry out steam sterilization.
Moist heat or heat saturated steam considered as the most effective sterilizing agent to sterilize glassware, culture media, surgical dressings, etc.
Time:
The minimal time requires to sterilize the contents in the gravity displacement autoclave, and pre-vacuum autoclave takes 30 minutes and 4 minutes, respectively, to destroy the microbial cells.
The sterilization time may vary depending on the type and load of the contents inside an inner chamber. The heavyweight of glassware, large liquid volumes, and dense materials may increase the sterilization time.
It is recommended that an autoclave should be operated preferably at high temperatures and short sterilization time over the combination of lower temperatures and longer sterilization time.
5. Components:
An autoclave is designed to work efficiently to destroy the structural proteins, enzymes, and spores of the microorganisms. Generally, there are two kinds of autoclave, one is gravity displacement, and the other is a pre-vacuum sterilizer.
The working of both the types will differ slightly. In gravity displacement type, the air is removed by a steam-activated exhaust valve, while in pre-vacuum type, the air is drained out via pulling the vacuum pump.
In both models, the air is replaced with pressurized steam at the desired temperature and time to maintain a sterile environment inside. So in this context, we will look into the basic components of the gravity displacement autoclave. The diagram of an autoclave illustrates the simplicity of operation.
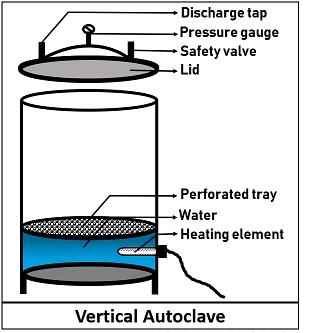
Pressure chamber:
It is the main body that comprises an inner chamber and an outer jacket. An inner chamber is composed of stainless steel, consisting of a tripod stand over which a perforated holding tray is placed. The materials to be sterilized are put over the holding plate.
An outer jacket used in medical setups is generally filled with steam that enters and passes through an operating valve. It flows forward and down through the chamber and reduces the time taken to reach the sterilization temperature. The capacity or size of pressure vessel ranges from 100 L to 3000 L.
Lid:
It is the second most crucial component of an autoclave that is provided with the following systems:
- Pressure valve: It regulates the pressure of the steam jacket and inner chamber.
- Safety valve: It is provided to protect from any damage to an autoclave due to overpressure.
- Exhaust valve: It is used to release steam.
- Whistle: It indicates that the pressure increased inside the vessel by lifting itself to release water vapours.
- Tightening knobs: There are some tightening knobs to lock the autoclave and forms a closed system to sterilize the goods.
Steam Generator:
Water is added into the inner chamber up to the level of the tripod stand. A power cable is attached to the heating rod that is required for steam production. A heating element or boiler is found at the bottom of the pressure vessel that uses a power supply to generate steam from the water.
The level of water is an essential factor that determines the efficiency of the steam sterilizer. There might get some chances of burning the heating element if the amount of water is too less. Similarly, more than enough water might damage the components placed inside.
6. Autoclaving:
Autoclaves are used extensively in practical labs, industries, healthcare settings to sterilize different kinds of equipment and media. The items are either wrapped or put directly over the holding plates inside an autoclave chamber under controlled conditions of temperature, pressure, and steam for a specific time.
The working of an autoclave is generally like a pressure cooker, which we use in our daily life to boil or cook the food. Like a pressure cooker, an autoclave has a door or lid that is tightened to form a sealed chamber. Then the air within the pressure vessel is displaced by many ways like steam, through steam flushes and vacuum systems depending upon the type of an autoclave.
After that, the pressure is applied to the steam that increases the temperature and killing ability to achieve successful sterilization at the desired time. Hence, the steam is exhausted after the completion of the sterilization, and thereby sterile equipment and media can be taken out. Therefore, depending upon the working of an autoclave, there are three phases in its sterilization cycle:
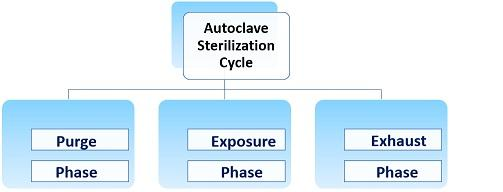
Purge Phase:
It also refers as the conditioning phase, in which the air inside the pressure vessel is displaced or removed that may inhibit the sterilization process. Different autoclaves use different methods to remove the air out of the chamber.
- Gravity displacement type autoclave: It uses steam to displace the air.
- Positive pressure displacement type autoclave: It uses steam flushes and pressure pulses.
- Negative pressure (vacuum) displacement type: It uses a vacuum pump to remove all the air.
Exposure Phase:
It also refers as the sterilization phase when the autoclave’s exhaust valve is closed, and the heating element provides continuous steam into the pressure vessel. It results a rapid increase in the temperature and pressure to the desired setpoint.
Then, the items placed inside the chamber meet the exposure phase, where they are held at sterilization temperature for the desired time depending upon the type and load of content.
Exhaust Phase:
It is the final phase when the exhaust valve is opened to release out the steam out of the chamber to depressurize the chamber so that the items on the tray can be taken out.
7. Advantages:
- Moist heat sterilization is a nontoxic and inexpensive method to carry out.
- Autoclave sterilizer provides a rapid microbicidal, sporicidal effect through its steam saturated with heat.
- Moist heat can penetrate into the fabrics more effectively instead of dry heat.
- Autoclave sterilizers are used in the food and industrial sites to maintain overall sterility by sterilizing the contents required in the process.
- Besides, it is also used in medical applications to sterilize medical equipment.
- In chemical industries, it is used to harden rubber and hydrothermal method.
8. Limitations:
- Moist heat sterilization might cause corrosion and combustion of lubricants.
- Some plasticware might melt under the high heat.
- Many chemicals breakdown during the sterilization process.
- The heat produced in autoclave takes much more time to sterilize solid media and large containers.
9. Conclusion:
Therefore, we can conclude that autoclave sterilization is the best way to sterilize culture media, pipette tips, equipment, glassware, etc. It is also useful to inactivate the bacteria, viruses, fungi, and yeasts, etc. in culture plates, medical and surgical wastes via autoclaving prior disposal.
Related Articles:
RELATED POSTS
View all